Part 3 of 4: Cycle of Painkiller Dependency
When used properly, painkillers can be a useful tool in aiding the recovery process. However, patients don’t always realize how dangerous and addictive painkillers can be, especially when they are prescribed by a healthcare provider. Many painkillers are opioids, mind-altering medications not intended for long-term use that often result in dependency or addiction.
When taking painkillers, the body’s nervous system is depressed, allowing for temporary pain relief and causing an abundant release of endorphins, your brain’s feel-good neurotransmitters. Endorphins muffle your perception of pain and boost feelings of pleasure, creating a temporary but powerful sense of well-being. Patients find themselves experiencing symptoms of withdraw and needing to regularly re-medicate, eventually leading to the need for more painkillers and higher doses to achieve the same feeling. This cycle of dependency has led to nearly 12 million Americans abusing painkillers daily and results in 130 opioid overdose deaths every day (Health Care Resource Centers, 2018).
The Cycle of Addiction
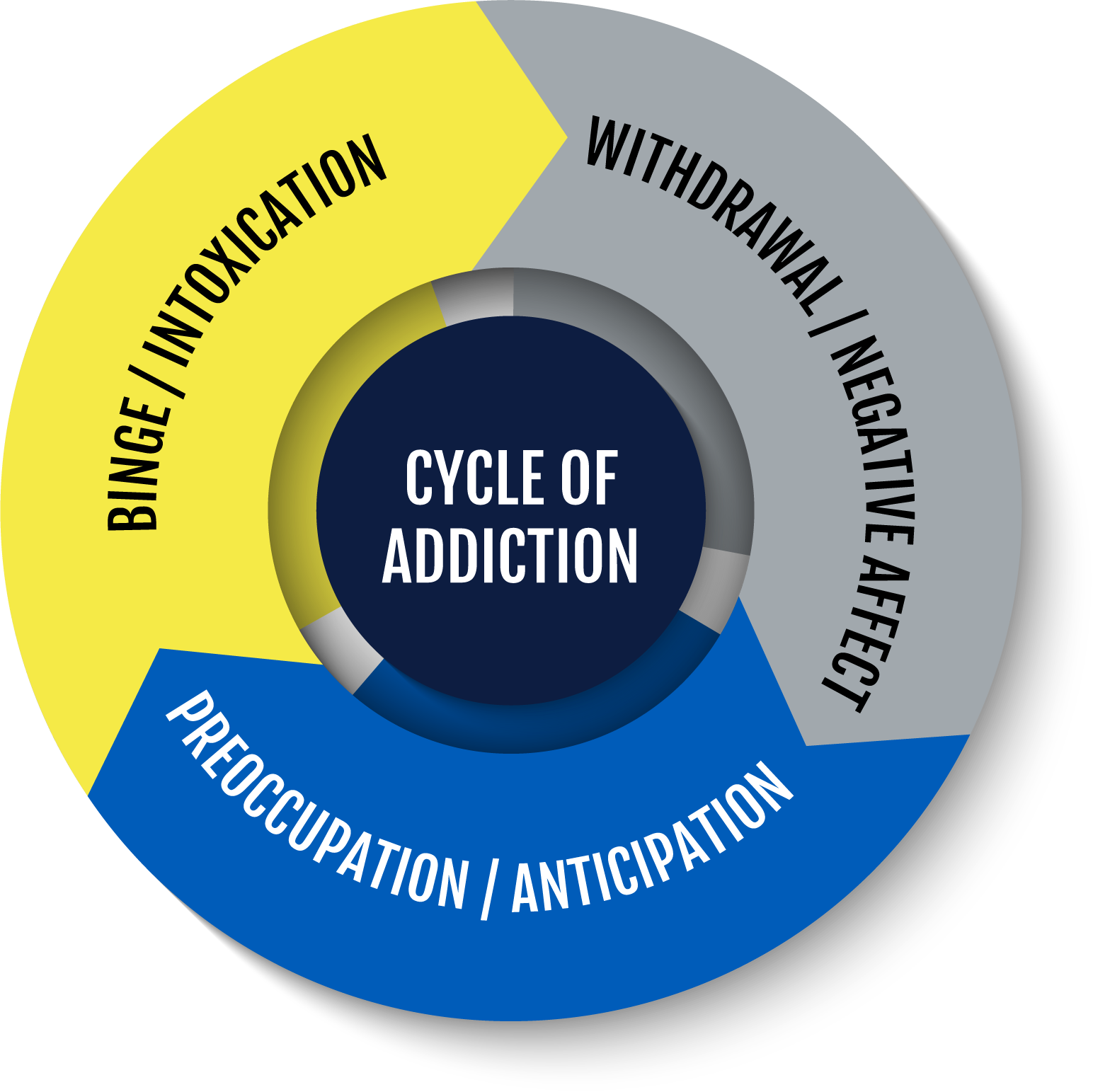
The cycle of addiction for all addictive substances can be broken into 3 primary categories: binge, withdrawal, and preoccupation. The cycle of painkiller addiction can be difficult to break due to the development of tolerances, increased use of medications, and dependency on the substance.
Binge/Intoxication: The starting point of the cycle when a patient begins use of painkillers. They achieve pain relief and experience a surge of endorphins as the painkiller suppresses proteins in the nervous system. Binges will become more demanding as tolerance to the painkillers increase.
Withdrawal/Negative Affect: The painkillers’ effects have worn off allowing pain to return and the feeling of euphoria to diminish. The time required between binge and withdrawal can shorten as tolerances are developed – the longer a patient stays in the cycle.
Preoccupation/Anticipation: The drive to re-medicate is powerful and manipulates decision making, causing the cycle to restart (Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US), 2016).
The Brain’s Response to Painkillers
“Feel-good” hormones, like dopamine and endorphins, are naturally occurring and act as a reward system for certain stimuli. Actions like eating and exercising cause a natural high, but any addictive substance can override natural stimuli with artificial ones.
The body’s opioid system consists of opioid receptors (mu, delta, kappa) and opioid hormones (endorphins, enkephalins, and dynorphins) that are naturally activated in response to pain or stress. When painkillers are introduced to the opioid system, they join opioid hormones in a surge of activity attaching themselves to opioid receptors. This sets off a chain of chemical reactions in the nervous system. Some neurons are locked down to prevent pain signals from reaching the brain, while other parts of the nervous system are turned on flooding the brain with dopamine (Medicurito, 2019).
The brain eventually adjusts to these surges, reducing its own output of dopamine and opioid hormones and relying more on painkillers to numb pain and feel good. Due to the reduced output of natural hormones, the body feels the effects of withdrawal when the surge of painkillers slows down and stops. The body becomes hypersensitive to stimuli, especially in the area experiencing pain, and can no longer support its own needs driving patients to seek out more painkillers to return to a feeling of ‘normal’ again.
The Mind-Altering Effects
During withdrawal, patients can experience negative emotions and physical symptoms like pain, bodily discomfort, fear, anxiety, sweating, and sometimes in extreme cases, seizures. These feelings are caused by the user’s nervous system overcompensating from the surge of opioids and struggling to find a chemical balance.
As dopamine levels in the brain decrease, the ability for the patients to properly prioritize tasks and make decisions becomes depressed, driving them to seek to maintain the levels of pleasure the brain has become accustomed to. With long-term use, a patient may no longer suffer from the initial physical pain that created the need for pain relief, but will still exhibit a strong desire to use opioids in order to feel “normal” (Julie Le Merrer, 2009).
Long-term users feel an overall reduction in sensitivity to the brain’s reward system from both naturally and artificially influenced hormones. The frequent activation of the brain’s reward system changes the way a person perceives stimuli. Feelings of pleasure derived from former hobbies and activities become dull, leaving the high from painkillers as the only outlet. Likewise, being around certain people, places, situations, or even emotional states can serve as triggers to seek out opioids despite lacking a negative feeling. Attempts to regain and maintain feelings of pleasure escalate as the body continuously adapts to the opioid surges. Ultimately, users feel encouraged to seek out more and stronger opioids, opening the door to illicit drug use and abuse.
Opioid Use Disorder and Quitting
Painkiller addiction is known as Opioid Use Disorder and those suffering from Opioid Use Disorder can include your family, friends, and colleagues. It is important that you provide a strong support network to those suffering from Opioid Use Disorder to help identify and treat their addiction. Signs that someone has an opioid addiction include:
- Consistent, long-term use of painkillers
- Poor decision making or out of character behavior
- Mood swings that seem like personality changes
- Changes in sleep pattern or inability to sleep
- Digestive distress, especially during withdrawal periods
- Borrowing, “losing”, hiding, or seeking more prescriptions for painkillers from various doctors (Detox & Recovery Network, 2019)
Recovery from Opioid Use Disorder is a hard battle and attempts to quit without intervention are often unsuccessful. Just as the user developed a tolerance to painkillers over time, they are going to need time to break the cycle of habitual use as well. Despite an absence of painkillers, the body is still operating at a lower level in anticipation to compensate for painkillers being reintroduced into the system. The good news is that the body learns to stop anticipating opioid surges after a period of just a few weeks to a few months. Weening off painkillers – reducing the dosage and/or extending the time between use – can be a good strategy to minimize the effects of withdrawal. During this period, the user should be physically active and take steps to rediscover activities and hobbies that bring them joy. This promotes a natural boost in dopamine and endorphins to help the body replace the high once felt with painkillers. Finding this natural balance can reduce the risk of relapse and improve quality of life.
Reach Out!
Get in touch with someone that can help. The Substance Abuse and Mental Health Services Administration (SAMHSA) operates a 24/7, year-round hotline for patients and families looking for help. Call SAMHSA: 1-800-662-4357.
To find local rehab centers, counseling, and support groups in Arizona, visit Start Your Recovery.org or the SAMHSA Opioid Treatment Program Directory.
Physical therapy can also be helpful in reducing opioid use by addressing pain, improving quality of life by increasing mobility and independence, and taking a natural approach to injury recovery. In fact, research shows that patients who see a physical therapist to address their pain take less opioids and for a shorter period of time than those who do not. This helps significantly reduce the risk of painkiller dependency (American Physical Therapy Association, 2021).
Learn more about Orthopedic Rehabilitation at Spooner. Ready to schedule an appointment? Schedule an appointment or complimentary movement screen with a Spooner physical therapist at one of our locations throughout the valley.
Resources:
- American Physical Therapy Association. (2021, Auguet 11). Physical Therapy vs Opioids: When to Choose Physical Therapy for Pain Management. Retrieved from ChoosePT: https://www.choosept.com/health-tips/physical-therapy-vs-opioids-when-to-choose-physical-therapy-pain-management
- Detox & Recovery Network. (2019, February 18). Overcoming the Opioid Use Cycle: Chronic Pain, Mental Health and Recovery. Retrieved from Guardian Recovery Network: https://www.guardianrecoverynetwork.com/addiction-detox-aftercare-planning/overcoming-the-opioid-use-cycle-chronic-pain-mental-health-and-recovery/
- Health Care Resource Centers. (2018, July). Opioid Addiction. Retrieved from Health Care Resource Centers: https://www.hcrcenters.com/opioid-addiction/
- Julie Le Merrer, J. A. (2009). Reward Processing by the Opioid System in the Brain. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4482114/: Physiol Rev.
- Medicurito (Director). (2019). Opioid Drugs, Part 2: Addiction and Overdose [Motion Picture].
- Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). (2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health . Washington DC: US Department of Health and Human Services.